The Real Connection Between IBS and What You Eat
Irritable bowel syndrome (IBS) can be a frustrating and often misunderstood condition. Many sufferers feel dismissed, their symptoms attributed simply to stress. But IBS is far more complex, involving intricate physiological processes within the gut. What you eat plays a significant role in managing, and sometimes even triggering, IBS symptoms.
One key factor is the gut-brain connection. This complex communication network links your emotional well-being with your digestive function. For example, high stress levels can worsen IBS symptoms by changing gut motility and increasing sensitivity to pain. This connection highlights why personalized IBS diet plans are often more effective than medication for managing the condition. You might be interested in: our blog categories.
Exploring the Science Behind IBS
Recent research is uncovering the mechanisms behind IBS. Intestinal permeability, sometimes called "leaky gut," occurs when substances that shouldn't pass through the intestinal lining. This can trigger inflammation and contribute to IBS symptoms. Disruptions in the microbiome, the complex community of bacteria in your gut, can also increase inflammation and alter digestion.
Another critical factor is visceral hypersensitivity. This means the nerves in the gut are more sensitive, causing individuals with IBS to experience pain more intensely. This explains why certain foods can trigger strong reactions in some people but not others. Globally, IBS affects a significant portion of the population. Studies estimate that between 10% and 20% of people worldwide suffer from IBS, with a global prevalence of approximately 11.2% reported in recent studies. This condition significantly impacts healthcare costs and is often treated with dietary changes like the low FODMAP diet. Learn more about IBS prevalence and treatment.
Beyond Diet: Other Helpful Strategies
While diet is crucial, other strategies can help manage IBS. Some individuals explore alternative therapies such as CBD for Irritable Bowel Syndrome. Recognizing these interconnected factors emphasizes the importance of a multifaceted approach. Addressing stress, supporting a healthy microbiome, and reducing intestinal permeability are also vital for long-term relief. This holistic approach empowers individuals to regain control of their digestive health and improve their overall well-being.
Mastering the Low FODMAP Approach Without Losing Your Mind
The low FODMAP diet has become a key part of IBS management, providing relief for many. This approach involves temporarily reducing FODMAPs (fermentable oligo-, di-, mono-saccharides and polyols), which are carbohydrates that can be hard to digest. Successfully following a low FODMAP diet takes planning and understanding.
Understanding the Elimination and Reintroduction Phases
The low FODMAP diet isn't about avoiding certain foods forever. It has two main parts: elimination and reintroduction. The elimination phase, usually 2-6 weeks long, involves severely limiting high FODMAP foods. This helps lessen symptoms and creates a baseline for finding trigger foods. Common culprits like onions, garlic, wheat, and dairy are avoided during this phase. This diet has proven highly effective for managing IBS symptoms. It restricts FODMAPs, commonly found in foods like wheat, dairy, and certain fruits and vegetables. Research shows that 50% to 80% of people with IBS find their symptoms significantly improve on this diet, with some studies indicating a 75% success rate. By temporarily removing potentially problematic foods, individuals can figure out which FODMAPs bother them most and tailor their diet accordingly. Learn more about the effectiveness of low FODMAP diets.
After elimination, the reintroduction phase begins. This involves systematically adding back specific FODMAP groups, one by one, and watching for any returning symptoms. This helps pinpoint personal trigger foods. You might find you handle lactose fine, but fructose causes issues. This personalized information is essential for a long-term IBS diet plan that actually works.
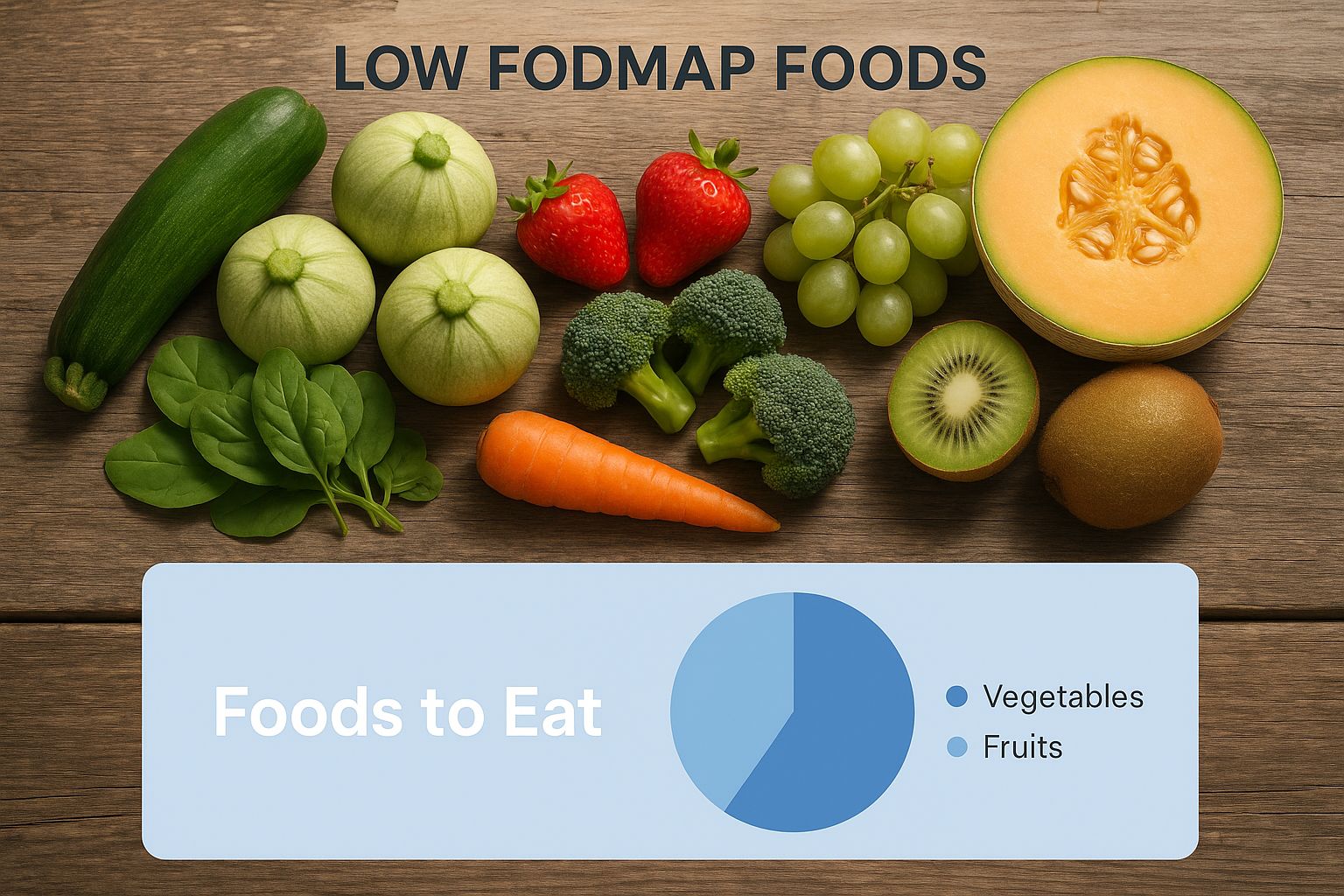
The image above shows various low FODMAP fruits and vegetables perfect for the elimination phase. These colorful, fresh choices prove a low FODMAP IBS diet can be enjoyable and nutritious, with plenty of tasty options. While this article focuses on alcohol, understanding how food affects how your body processes things is always helpful. For example, you might want to know about the best foods to eat before drinking.
Practical Tips for Low FODMAP Success
Following the low FODMAP diet requires planning and attention to detail. Carefully check food labels, as even small amounts of hidden FODMAPs can trigger symptoms. Also, look for low FODMAP recipes and online support groups for meal ideas and encouragement. This support can be incredibly helpful when you're starting out. Sticking to a low FODMAP diet can be challenging when eating out or traveling. Planning meals, checking restaurant menus, and packing low FODMAP snacks helps keep you on track and minimize discomfort.
To help you make smart food choices, here's a handy table:
High FODMAP Foods vs. Satisfying Low FODMAP Alternatives
This table compares common high FODMAP foods with suitable low FODMAP substitutes.
| Food Category | High FODMAP Foods to Avoid | Low FODMAP Alternatives |
|---|---|---|
| Dairy | Milk, yogurt, ice cream | Lactose-free milk, almond milk, hard cheeses |
| Fruits | Apples, pears, mangoes | Bananas, blueberries, strawberries |
| Vegetables | Onions, garlic, broccoli | Spinach, carrots, eggplant |
| Grains | Wheat, rye, barley | Oats, rice, quinoa |
| Sweeteners | Honey, high fructose corn syrup | Maple syrup, sucrose |
This table provides a quick guide for swapping high FODMAP foods for low FODMAP options, making the diet easier to follow. Remember to consult resources like the Monash University FODMAP app for the most comprehensive and up-to-date information.
Beyond FODMAPs: The Hidden Triggers Sabotaging Your Gut

While the low FODMAP diet is a cornerstone of many IBS diet plans, it isn't a universal solution. Many people experience lingering symptoms despite carefully restricting FODMAPs. This happens because other hidden triggers might be at play, impacting gut health and hindering progress. Let's explore these often-overlooked culprits.
Unveiling the Hidden Culprits
Several factors beyond FODMAPs can contribute to IBS symptoms. These include non-celiac gluten sensitivity, histamine intolerance, bile acid malabsorption, and reactions to food additives. Understanding these issues is vital for a truly effective IBS diet plan.
Non-celiac gluten sensitivity can mimic celiac disease symptoms without the same immune response. Even with a negative celiac disease test, gluten might still irritate your gut. Histamine intolerance can cause various symptoms, like digestive upset, headaches, and skin rashes. Because histamine is in many foods, identifying and limiting them can significantly improve well-being.
Another often-missed factor is bile acid malabsorption. Bile acids are essential for fat digestion, but if not absorbed properly, they can irritate the colon and cause diarrhea. Finally, food additives like artificial sweeteners and preservatives can trigger IBS symptoms in sensitive individuals. This is why focusing on whole, unprocessed foods is crucial for any successful IBS diet plan.
Identifying and Managing Hidden Triggers
Recognizing the signs of these hidden triggers is the first step in managing them. For instance, if symptoms worsen after eating gluten, even without celiac disease, non-celiac gluten sensitivity might be involved. A detailed food diary can help identify patterns and potential triggers.
- Food Diary: Track your food intake and any related symptoms to connect specific foods to IBS flares.
- Elimination Diet: With guidance from a healthcare professional or registered dietitian, temporarily remove suspected trigger foods to see if symptoms improve.
- Testing: Specialized tests can diagnose conditions like bile acid malabsorption.
Once potential triggers are identified, dietary modifications are key. This could mean avoiding gluten, limiting high-histamine foods, or reducing processed foods with additives. For bile acid malabsorption, medication can improve bile acid absorption. Working with a registered dietitian helps create a personalized IBS diet plan that addresses your unique triggers and needs. This targeted approach, considering both FODMAPs and other potential culprits, can lead to lasting relief and better IBS management. Furthermore, understanding your needs allows for a more flexible and less restrictive long-term IBS diet plan.
Crafting Your Personalized IBS Diet Plan That Actually Works
Generic dietary advice rarely helps those suffering from Irritable Bowel Syndrome (IBS) because triggers and tolerances are so individual. This section offers a personalized roadmap for developing an IBS diet plan that actually delivers results. It requires careful tracking, strategic food reintroductions, and understanding your body's unique responses.
Tracking Your Symptoms and Identifying Triggers
The first step towards a personalized plan is understanding your body's reactions to different foods. A detailed food and symptom diary is essential. Record everything consumed, noting the time and portion size. At the same time, track your IBS symptoms, including their severity and duration. For instance, if bloating occurs after eating a certain food, your diary will help connect the cause and effect. After a few weeks, clear patterns will start to emerge, revealing hidden links between specific foods and symptom flares. You might be interested in: How to master your diet.
Establishing Your Baseline Diet
Once you've identified potential trigger foods, it's time to establish a baseline diet. This diet minimizes symptoms and ensures proper nutrition. It usually involves temporarily removing common IBS triggers, even if they haven’t shown up in your diary yet. This elimination phase, typically lasting 2-6 weeks, creates a calmer gut environment for the next phase: reintroduction.
Reintroducing Foods Strategically
Strategically reintroducing foods is the key to pinpointing your specific triggers. Add one potential trigger food back into your diet at a time, in a small quantity. Carefully monitor your symptoms over the next 2-3 days. If symptoms reappear, you've identified a trigger. If not, you might tolerate that food. This process should be repeated for each potential trigger, one by one. Avoiding common testing errors, such as reintroducing multiple foods at once, is essential for accurate results. This method helps you build a list of safe and trigger foods, the foundation of your effective IBS diet.
Practical Meal Planning and Nutritional Balance
Armed with your personalized trigger list, you can begin planning nutritious meals that avoid problem foods. This often requires creative substitutions. For example, if onions are a trigger, try using onion-infused oil for flavor. Remember, a balanced diet is crucial, even with restrictions. A Registered Dietitian can be an invaluable resource to ensure your nutritional needs are met while managing IBS.

The following table provides a sample 3-day meal plan blueprint, showcasing low FODMAP options while emphasizing balanced nutrition. Remember to adapt this blueprint to your individual trigger foods and preferences.
3-Day Personalized IBS-Friendly Meal Plan Blueprint
| Day | Breakfast | Lunch | Dinner | Snacks |
|---|---|---|---|---|
| 1 | Gluten-free oatmeal with lactose-free milk and berries | Grilled chicken salad with mixed greens, cucumber, and tomatoes (dressing: olive oil and lemon juice) | Baked salmon with steamed green beans and brown rice | Lactose-free yogurt with a handful of almonds |
| 2 | Scrambled eggs with spinach and a slice of gluten-free toast | Turkey lettuce wraps with bell peppers and carrots | Chicken stir-fry with brown rice noodles and low FODMAP vegetables (e.g., bok choy, zucchini) | Rice cakes with peanut butter |
| 3 | Smoothie with lactose-free milk, banana, spinach, and protein powder | Leftover chicken stir-fry | Grilled steak with mashed sweet potatoes and steamed broccoli | Hard-boiled egg |
This meal plan offers a glimpse into how you can incorporate low FODMAP principles into your daily diet. Remember, this is just a starting point, and personalizing it to your specific needs and preferences is key.
Partnering with Healthcare Providers
Creating a successful IBS diet plan is a team effort. Your healthcare provider can provide guidance, rule out other conditions, and recommend additional therapies. Open communication about symptoms, trigger foods, and dietary challenges is essential for a holistic approach to IBS management. This collaborative approach empowers you to take control of your digestive health and improve your overall quality of life. This includes combining your personalized diet with other management strategies for a more comprehensive and effective treatment plan.
Making Your IBS Diet Plan Stick When Life Gets Real
Maintaining any dietary change is challenging. Sticking to an IBS diet plan amid daily life can feel especially daunting. This section addresses practical aspects of navigating social situations, meal prepping, and staying motivated while following a restrictive diet.
Navigating Social Events and Restaurants
Social events and restaurants often present the biggest hurdles for those following an IBS diet. With careful planning, you can enjoy these occasions without triggering symptoms. Before going to a restaurant, review the menu online and identify low FODMAP options. Don't hesitate to call ahead and ask about ingredients or special accommodations.
When attending social gatherings, offer to bring a dish you know is safe. This ensures you'll have at least one meal option that won't cause discomfort. Having a go-to list of safe foods generally available at most restaurants—like grilled fish or chicken and steamed vegetables—can simplify ordering.
Meal Prepping for IBS Success
Efficient meal prepping is crucial for maintaining an IBS-friendly diet. Preparing meals and snacks in advance reduces the temptation of convenient, but potentially triggering, foods. Designate a specific day each week for meal prep. Focus on simple, low FODMAP recipes that can be easily stored and reheated.
This might include batch-cooking quinoa, roasting vegetables, or grilling chicken breasts. Preparing grab-and-go snacks like hard-boiled eggs or lactose-free yogurt with berries also helps avoid impulsive food choices when you're hungry.
Decoding Food Labels
Becoming a savvy label reader is crucial for an IBS diet. Many processed foods contain hidden triggers, like high fructose corn syrup or inulin. Carefully examine ingredient lists and look for FODMAPs hiding under different names. For example, "natural flavors" can sometimes contain onion or garlic powder.
Even products marketed as "healthy" may contain ingredients that aggravate IBS symptoms.
The Psychological Side of Dietary Management
Managing IBS isn't just about the food you eat. Stress can significantly worsen symptoms, highlighting the importance of mental well-being. Mindful eating practices can help reduce stress around meals. Focus on savoring each bite and paying attention to your body's hunger and fullness cues.
This can reduce the likelihood of overeating, which can trigger IBS symptoms. Setbacks are inevitable. Don't let occasional slip-ups derail your progress. View them as learning opportunities and recommit to your IBS diet the next day.
Expanding Your Diet Gradually
After the initial restriction phase of your IBS diet, you can gradually reintroduce foods to identify your specific triggers. This process involves adding back one FODMAP group at a time, in small amounts, while monitoring your symptoms. This systematic approach allows you to personalize your diet and broaden your food choices while maintaining symptom control.
Dietary management is a journey, not a destination. By implementing these strategies, you can create a sustainable IBS diet that works for your lifestyle and helps you regain control of your digestive health.
Beyond Diet: Powerful Complementary Strategies for Relief
A well-structured IBS diet plan is essential for managing Irritable Bowel Syndrome. However, relying solely on diet may not be enough to achieve complete symptom control. That's where complementary strategies come into play. These additional approaches work in tandem with your diet to enhance relief and improve your overall well-being.
Gut-Directed Hypnotherapy and Stress Management
The connection between the gut and the brain is a key factor in IBS. Gut-directed hypnotherapy has emerged as a promising therapy for reducing IBS symptoms. It works by targeting the gut-brain axis, helping to regulate gut function and reduce visceral hypersensitivity, a heightened sensitivity in the gut. Research suggests that for some individuals, this type of hypnotherapy can be even more effective than medication.
In addition to hypnotherapy, managing stress is crucial for IBS sufferers. Stress can significantly worsen symptoms. Incorporating practices like mindfulness, yoga, and deep breathing exercises can help manage stress and its negative impact on the gut. These techniques promote relaxation, potentially reducing the frequency and intensity of IBS flares.
Targeted Supplements: Peppermint Oil, Probiotics, and Digestive Enzymes
Specific supplements can offer additional support for managing IBS. Peppermint oil has been shown to alleviate abdominal pain and bloating. It works by relaxing the muscles in the digestive tract. Choosing enteric-coated peppermint oil capsules is important to prevent heartburn.
Probiotics, especially certain strains like Bifidobacterium infantis and Lactobacillus plantarum, can help restore balance to the gut microbiome. A balanced microbiome promotes better digestion and reduces inflammation, which can alleviate IBS symptoms.
Digestive enzymes can also be beneficial, especially for those who have difficulty digesting certain carbohydrates. These enzymes can aid digestion and reduce gas production, a common IBS symptom. For more information on managing carbohydrate intake, you might be interested in: How to master a low FODMAP diet.
Lifestyle Modifications: Physical Activity, Sleep, and Hydration
Beyond targeted therapies and supplements, simple lifestyle changes can significantly impact IBS. Regular physical activity helps regulate bowel movements and reduce stress. Aim for at least 30 minutes of moderate-intensity exercise on most days of the week.
Quality sleep is also essential. Inadequate sleep can disrupt gut function and exacerbate IBS symptoms. Prioritizing 7-8 hours of uninterrupted sleep each night can support good digestive health.
Finally, maintaining sufficient hydration is crucial for optimal gut function. Drinking plenty of water throughout the day can help prevent constipation and encourage regular bowel movements.
Integrating Complementary Strategies for Optimal Relief
By combining these complementary strategies with your IBS diet plan, you can develop a comprehensive approach to managing your symptoms. Remember, these strategies are most effective when used together. For example, combining a low FODMAP diet with stress management techniques and gut-directed hypnotherapy can provide more substantial relief than relying on a single approach. Success stories highlight the positive impact of this integrated approach, offering hope and improved quality of life for those with IBS.
Fuel your gut health journey with Cantein's premium plant-based protein and snacks, designed for optimal digestion and overall well-being. Visit Cantein today to explore our product range and discover how they can support your IBS diet plan.

